More than half of the people in the US living with HIV are 50 years old and older. With the use of antiretroviral medications, people who were diagnosed with HIV decades ago have been able to live well into older adulthood. This is great news.
Sadly, stigma due to age, sexual orientation, gender identity, and HIV status contributes to poor mental health and physical health.
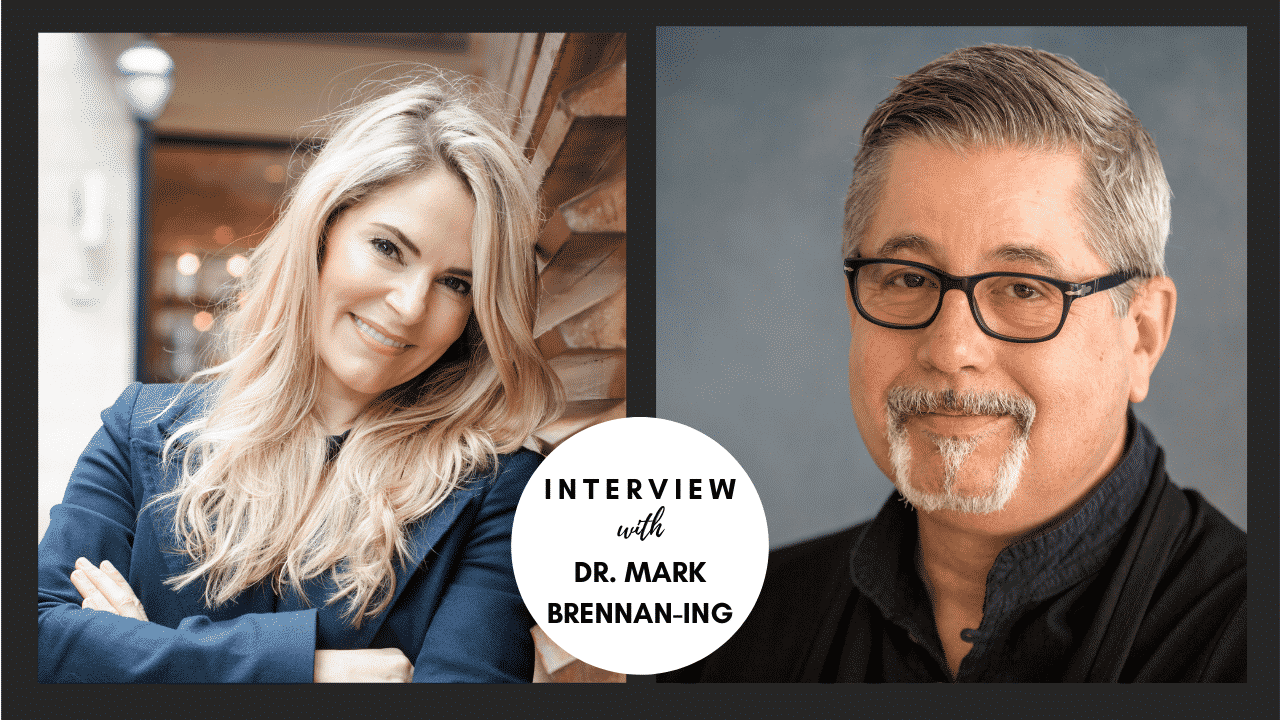
In this interview, Dr. Mark Brennan-Ing, Director of Research and Evaluation at the Brookdale Center for Healthy Aging at Hunter College, the City University of New York is on the Psychology of Aging podcast sharing important information about:
- HIV among people aged 50 and over
- The social, cultural, and medical reasons that adults 55 and older live with HIV longer before getting a diagnosis
- Reasons why people living with HIV might be experience depression at 5 times that of the general population
- What we can do to help meet the medical and mental health needs of aging adults with HIV
Here’s a peek inside the interview:
- [05:15] HIV among people aged 50 and over is on the rise in the US and the world. Learn more about the aging of the HIV epidemic.
- [07:41] How is antiretroviral therapy helping people to live longer?
- [14:08] What is Pre-exposure prophylaxis (or PrEP)? Does it really work?
- [20:48] What are the social, cultural, and medical reasons that adults 55 and older live with HIV longer before getting a diagnosis?
- [26:46] What is “inflammaging” and how does it intersect with HIV?
- [30:17] How does stigma affect people living with HIV?
- [32:53] People living with HIV experience depression at 5 times that of the general population. Learn some of the reasons why.
- [43:37] What can we do to help meet the medical and mental health needs of aging adults with HIV?
- [47:02] People living with HIV have incredible reserves of resilience and survivorship. Learn more about how to resilience to promote mental wellness in people living with HIV?
Watch a video clip of our interview, here:
AboutMark Brennan-Ing, PhD
Mark Brennan-Ing, PhD, is a Director of Research and Evaluation at the Brookdale Center for Healthy Aging at Hunter College, the City University of New York. Dr. Brennan-Ing’s research focuses on psychosocial issues affecting persons living with HIV and older sexual minority and gender diverse adults. They are Past-President of the State Society on Aging of New York (SSANY), a Fellow of the Gerontological Society of America (GSA), a Fellow of Division 44 (Psychology of Sexual Orientation and Gender Diversity) of the American Psychological Association, and past Board Member of the New York Association on HIV over Fifty (NYAHOF). They were the Principal Convener for GSA’s HIV/AIDS and Aging interest group, a member of the American Society on Aging’s LGBT Aging Information Network Leadership Council, and 2016 Chair of the American Psychological Association’s Committee on Sexual Orientation and Gender Diversity. They were an invited member of the NIH Office of AIDS Research Working Group on HIV and Aging in 2011. Dr. Brennan-Ing has been recognized for their work by the Hunter-Brookdale Center on Aging, Pride Senior Network, and the New York State Office for the Aging. In 2017 they received the Walter M. Beattie Award from SSANY. Dr. Brennan-Ing was the lead editor of Older Adults with HIV: An In-depth Examination of an Emerging Population (2009), and the 2016 volume, HIV and Aging: Interdisciplinary Topics in Gerontology and Geriatrics (vol. 42), which received a “High Commendation” from the British Medical Association. They have authored over 100 peer-reviewed articles, chapters and books.
Important Note:
People aged 50 and older need to know their HIV status so they can take medicine to treat HIV if they have the virus. Taking HIV medicine every day can make the viral load undetectable. People who get and keep an undetectable viral load (or stay virally suppressed) can live a long and healthy life. They also have effectively no risk of transmitting HIV to HIV-negative sex partners. – Centers for Disease Control & Prevention
Learn more about memory loss
If you’re concerned about someone you love possibly having a significant memory loss or a dementia disorder, please download my free memory loss guide. It answers some of the most frequently asked questions I get about memory loss.
Mentioned in this episode:
- CDC’s Pre-Exposure Prophylaxis (PrEP) information page
- CDC’s HIV and Aging information page
Resources for LGTBQ Older Adults
- SAGEConnect links LGBT elders with their broader community, reducing isolation and promoting well-being- connect online here. If you know someone who would benefit from SAGEConnect, but doesn’t have internet, call the registration line at 929-484-4160.
- Check out SAGE’s LGBTQ Aging Guides and Resources
- Considering Long-Term Care? Check out these resources for LGTBQ seniors
- Facing discrimination in your senior community? Lambda Legal defends the rights of LGBT and HIV-positive seniors who face discrimination related to their sexual orientation, gender identity or HIV status, including discrimination by staff and residents at senior centers, senior housing, long-term care and beyond.