A couple of weeks ago, I got together (over Zoom, of course) with my dear friend, Psychologist, Dr. Quiera Lige. She shared with me that she had an older family member who would benefit from therapy, but that this family member had not known any other people in their generation to go to to therapy and didn’t know what to expect. She suggested that I create a podcast episode about what therapy actually looks like when you go to therapy as an older adult.
For older adults, there is a lot of stigma surrounding what it means to need mental health care and as a result, older adults do not tend to seek out therapy when they need it.
Older adults continue to experience mental health concerns as they age. Studies show that when older adults do engage in mental health care, the vast majority of the time they get better.
If we can help older adults who are struggling with depression, anxiety, insomnia, grief, compounded loss, trauma, medical problems – you choose, get to that first therapy session, they’re one step closer to feeling better and living a more peaceful life.
My hope is that this episode will demystify the process of going to therapy and build a bridge from suffering to healing.
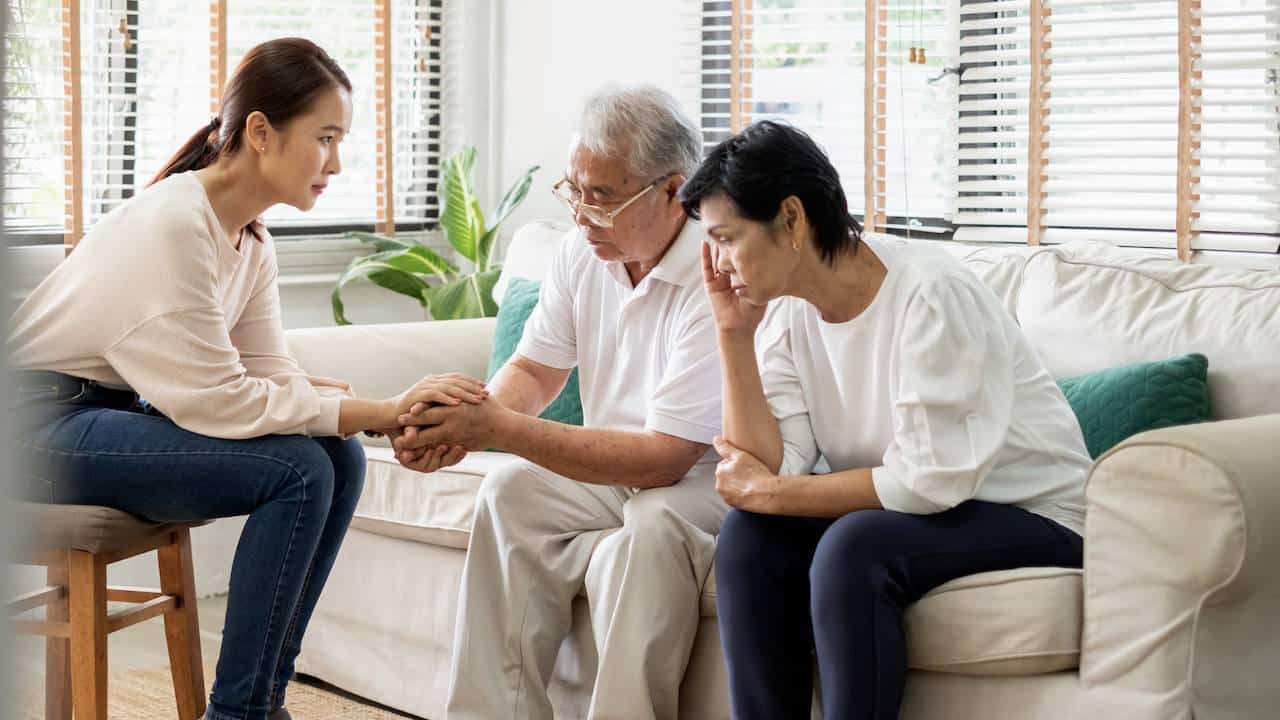
Today’s episode focuses on what a first therapy session may look like if you’re an older adult with a mental health concern, a memory concern, or a family concern.
Here’s a peek inside the episode:
- [01:37] Making the decision to schedule that first mental health appointment generally takes a lot of thought and courage. Learn what I hope you get from this episode.
- [04:11] Many therapists are taking COVID precautions very seriously and offering tele-therapy. I discuss how to talk with your therapist about COVID safety.
- [07:57] Some of the first objections that I hear from older adults when starting therapy is: “I don’t want you to think I’m crazy.” Or, “I don’t want you to lock me up”. If you’re considering starting therapy, it’s important to know the informed consent process , meaning, the specific situations that I would need to break confidentiality to get you support.
- [12:19] I ask a lot of questions in a first session to get to know my client’s current concerns and about my client’s life. I reveal many of the questions I ask in a first session,
- [16:59] Wonder what I do when people share concerns about memory loss in a first session? I describe my process here.
- [20:59] What does a first session look like when family members come to therapy with a person with dementia? Learn more here.
- [24:29] It’s okay and encouraged to ask your therapist questions. I share questions to consider asking.
- [26:32] You’re not gonna click with everyone. I share what happened when I didn’t connect with a therapist I was just getting started with.
If you or someone you know is in crisis or struggling with thoughts about harming yourself or others, please reach out to the National Suicide Prevention Lifeline.